insulin injection bottle
Understanding Insulin Injection Bottles A Guide for Diabetic Patients
For individuals living with diabetes, managing blood sugar levels is a daily task that often requires the use of insulin. Insulin therapy has proven to be effective for many, helping to regulate glucose levels in the body. A crucial component of this therapy is the insulin injection bottle. Understanding how to properly use these bottles is vital for ensuring effective treatment and maintaining overall health.
What is an Insulin Injection Bottle?
An insulin injection bottle, commonly known as a vial, is a container designed to hold insulin in liquid form. These bottles are typically made of glass or plastic and are sealed to maintain sterility. Insulin is available in various concentrations and types, including rapid-acting, long-acting, and intermediate-acting formulations. Patients must know which type of insulin they are prescribed to ensure they are using the correct product.
The insulin inside these bottles is sensitive to temperature and light. It should be stored in a cool place, away from direct sunlight, and never frozen. Proper storage is essential for maintaining the potency and effectiveness of the insulin.
Drawing Insulin from the Bottle
When using an insulin injection bottle, proper technique is important. Before drawing insulin, patients should wash their hands thoroughly to minimize the risk of introducing bacteria. If the vial contains cloudy insulin, it should be gently rolled between the palms to mix, rather than shaken, to avoid bubble formation.
To administer insulin from a vial, a syringe is typically used. The following steps should be followed
1. Prepare the syringe by pulling back on the plunger to the appropriate dosage mark. 2. Insert the needle into the rubber stopper of the vial. 3. Push the plunger down to inject the air into the vial. This creates a vacuum, making it easier to draw out the insulin. 4. Invert the vial while keeping the needle in it, and pull back the plunger to draw the prescribed amount of insulin into the syringe. 5. Check for air bubbles in the syringe. If any are present, they can be removed by tapping the syringe and pushing the plunger slightly to expel the air. 6. Finally, withdraw the needle from the vial, and the insulin is ready for injection.
insulin injection bottle
Administering the Injection
Once the insulin is drawn into the syringe, it is time to administer the injection. Patients should rotate injection sites to prevent lipodystrophy, a condition that can occur with repeated injections in the same area. Common sites for insulin injections include the abdomen, thighs, and upper arms.
To inject insulin
1. Clean the injection site with an alcohol swab. 2. Pinch the skin to lift it away from the muscle beneath. 3. Insert the needle at a 90-degree angle (or 45 degrees for those with less body fat). 4. Push the plunger down slowly to inject the insulin. 5. Remove the needle and apply gentle pressure to the site for a few seconds. 6. Dispose of the syringe in a sharps container.
Monitoring Blood Sugar Levels
After administering insulin, it's crucial for patients to monitor their blood sugar levels regularly. This helps assess how well the insulin is working and whether any adjustments in dosage or timing are necessary. Continuous Blood Glucose Monitors (CGMs) can provide real-time data, allowing for more effective management of diabetes.
Conclusion
Insulin injection bottles are essential tools in diabetes management. Understanding how to properly use these bottles, draw insulin, and administer injections can greatly enhance a patient's ability to control their blood sugar levels. By following best practices and maintaining open communication with healthcare providers, individuals with diabetes can lead healthy, active lives. Ultimately, knowledge and confidence in using insulin injections empower patients in their journey towards effective diabetes management.
-
Aesthetic Makeup Spray Bottles | Fine Mist Empty RefillableNewsAug.19,2025
-
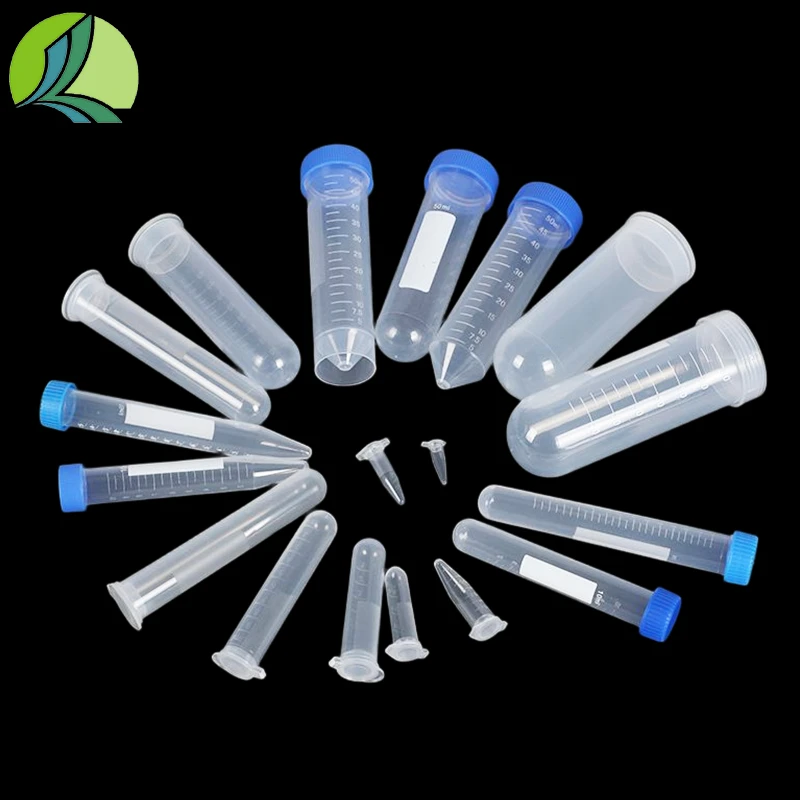
White Plastic Veterinary Vaccine Vials | Lab Liquid BottlesNewsAug.18,2025
-
Plastic Medicine Liquid Bottle: Secure Flip Top Drug VialsNewsAug.17,2025
-
Durable 250ml Blue Plastic Vaccine Vial for Lab & Vet UseNewsAug.16,2025
-
Sterile Virus Sample Tubes: Secure & Reliable Specimen CollectionNewsAug.15,2025
-
White 250ml Plastic Vaccine Vial for Lab & Vet MedicineNewsAug.14,2025