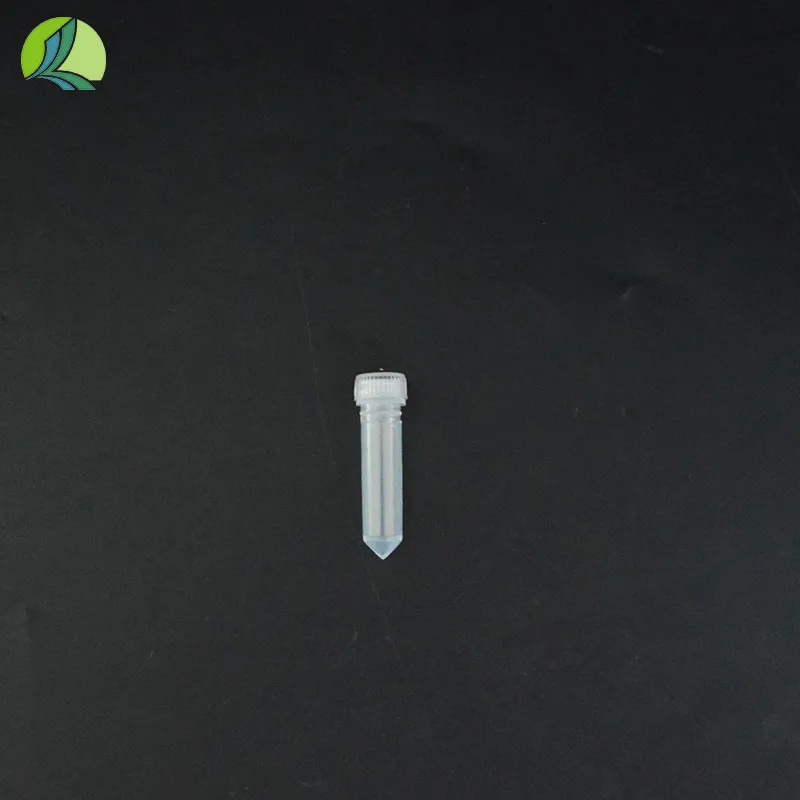
plain serum tube
Understanding Plain Serum Tubes A Vital Component in Clinical Laboratory Testing
In the realm of clinical laboratories, the importance of sample collection and transport cannot be overstated. Among the various types of specimen containers, the plain serum tube stands out as a vital component in the process of blood sample analysis. These tubes are specifically designed to facilitate the collection of serum, which is the liquid portion of blood that remains after coagulation. Understanding the characteristics, usage, and significance of plain serum tubes can greatly enhance laboratory efficiency and the accuracy of diagnostic testing.
Plain serum tubes are typically made from glass or plastic, and they feature a simple design with no additives that promote clotting or prevent it. This lack of anticoagulants allows blood samples to clot naturally when the tubes are inverted or left standing at room temperature. Once coagulation occurs, the liquid serum can be easily separated from the cellular components of the blood through centrifugation.
One of the key aspects of using plain serum tubes is their specific use in serological tests, hormone level assessments, and various biochemical analyses. For instance, tests that measure electrolyte levels, enzyme activities, and other biomarkers commonly utilize serum obtained from these tubes. The absence of anticoagulants means that the results are not influenced by any substances that could potentially alter the biochemical composition of the serum, leading to more accurate and reliable test outcomes.
plain serum tube

To collect a blood sample in a plain serum tube, healthcare professionals typically perform venipuncture, inserting a needle into a vein and allowing the blood to flow into the tube. It is crucial that the tube is properly labeled, indicating the patient's information and the type of test required. Once the sample is collected, the tube must be gently inverted to mix the clotting factors, followed by allowing it to stand for a specified period. This time frame allows the blood to clot, after which the tube is placed in a centrifuge for separation.
The proper handling and processing of plain serum tubes are essential to minimize contamination and ensure the integrity of the specimen. Healthcare providers should observe protocols concerning storage conditions, such as temperature control, to preserve the serum's stability. Additionally, it is vital to adhere to the laboratory's guidelines regarding the time interval between sample collection and analysis. Delays in processing can lead to hemolysis or degradation of the serum, which may impact the results of tests.
In recent years, advancements in technology and materials have led to the development of various types of serum tubes tailored for specific testing needs. Some plain serum tubes may feature specialized closure systems or coatings that further reduce the risk of contamination. These innovations aim to enhance the safety and reliability of serum sample collection, directly impacting patient care and treatment decisions.
In conclusion, plain serum tubes play a pivotal role in the field of clinical diagnostics. Their straightforward design allows for the collection of high-quality serum samples, which are crucial for a wide range of laboratory tests. As the healthcare landscape continues to evolve, understanding the significance of these tubes and adhering to best practices in their use will remain fundamental to ensuring accurate diagnoses and effective patient management. In the end, the humble plain serum tube is a small but critical player in the larger framework of modern medicine, underscoring the importance of proper sample collection and processing in delivering quality healthcare.
-
Aesthetic Makeup Spray Bottles | Fine Mist Empty RefillableNewsAug.19,2025
-
White Plastic Veterinary Vaccine Vials | Lab Liquid BottlesNewsAug.18,2025
-
Plastic Medicine Liquid Bottle: Secure Flip Top Drug VialsNewsAug.17,2025
-
Durable 250ml Blue Plastic Vaccine Vial for Lab & Vet UseNewsAug.16,2025
-
Sterile Virus Sample Tubes: Secure & Reliable Specimen CollectionNewsAug.15,2025
-
White 250ml Plastic Vaccine Vial for Lab & Vet MedicineNewsAug.14,2025