Understanding the Importance of Plain Serum Tubes in Clinical Laboratory Testing and Sample Collection
Understanding the Role of Plain Serum Tubes in Clinical Diagnostics
In the realm of clinical diagnostics, the importance of sample collection and processing cannot be overstated. One of the critical components of this process is the use of plain serum tubes, often referred to as PSTs (Plain Serum Tubes). These tubes are vital for collecting blood samples that will be used for a variety of laboratory tests. This article explores the significance, design, and application of plain serum tubes in a clinical setting.
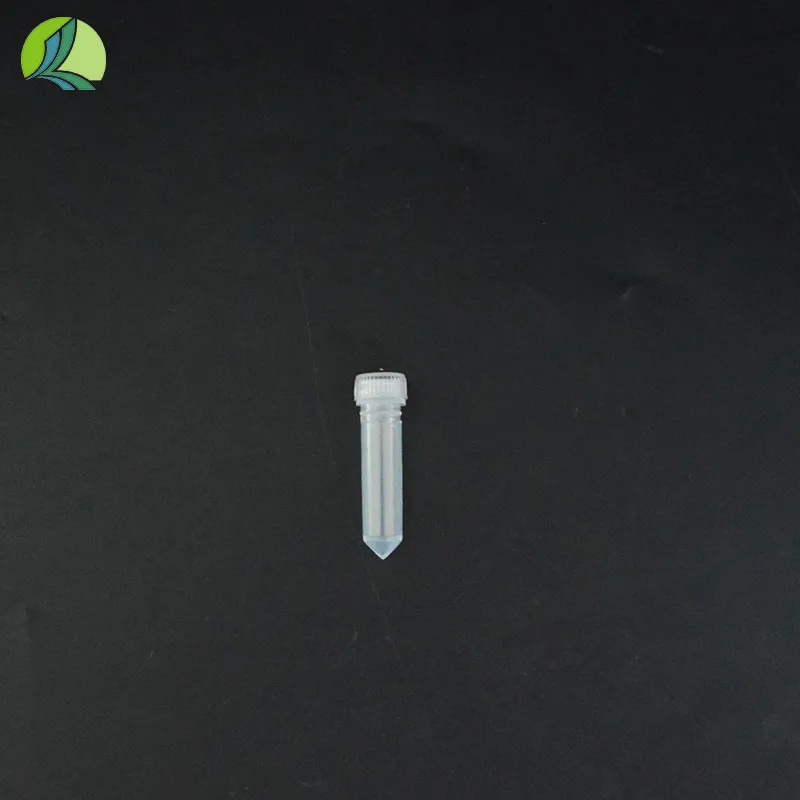
What Are Plain Serum Tubes?
Plain serum tubes are blood collection containers that do not contain any anticoagulants or additives. Typically made from glass or plastic, these tubes allow blood to clot naturally after collection. The design usually features a stopper, which may be colored to indicate the type of tube and its intended use. Once the blood has clotted, it is then centrifuged, resulting in the separation of serum from the cellular components of the blood. The serum, which is a clear liquid, contains valuable biomarkers that can be analyzed for various medical conditions.
Importance in Diagnostics
Plain serum tubes are primarily used for tests that require serum rather than whole blood. Many biochemical assays, serological tests, and hormonal evaluations are performed on serum samples. The accuracy and reliability of the results depend heavily on the quality of the collected samples. Using plain serum tubes ensures that the samples are free from anticoagulants that could interfere with certain laboratory tests.
For instance, tests that measure electrolyte levels, liver function tests, and cardiac markers often utilize serum samples collected in plain tubes. The absence of anticoagulants is crucial in these cases since any additives could potentially skew results, leading to misdiagnosis or improper treatment recommendations.
plain serum tube

Proper Collection Technique
To ensure optimal results, proper collection and handling techniques for plain serum tubes are crucial. Blood should be drawn using a sterile technique, and the collection should be done with care to minimize hemolysis (destruction of red blood cells) or contamination. After blood collection, the tubes are often gently inverted to mix, ensuring even distribution of components. It is essential to allow the blood to clot at room temperature for the appropriate duration before centrifugation. The standard clotting time is usually between 20 to 30 minutes.
Centrifugation and Serum Analysis
Once clotting has occurred, the tubes are placed in a centrifuge. Centrifugation separates the serum from clotted blood cells due to the differences in density. The resulting serum can then be carefully pipetted off for analysis while avoiding disturbance to the clot, thus preventing contamination. It is critical to process these samples in a timely manner, as prolonged storage can lead to degradation of serum components.
Challenges and Considerations
While plain serum tubes are beneficial for many tests, they do present challenges. For example, incorrect storage temperatures or delays in processing can affect sample integrity. It is essential for laboratories to adhere to strict protocols for sample handling, transport, and analysis to maintain quality control.
In conclusion, plain serum tubes are indispensable in the field of medical diagnostics. Their design facilitates the collection and processing of clean serum samples essential for a range of laboratory tests. As the healthcare industry evolves, ongoing education regarding best practices in blood collection and sample processing remains vital to ensure accurate diagnostic outcomes and ultimately improve patient care.
-
Durable 250ml Blue Plastic Vaccine Vial for Lab & Vet UseNewsAug.16,2025
-
Sterile Virus Sample Tubes: Secure & Reliable Specimen CollectionNewsAug.15,2025
-
White 250ml Plastic Vaccine Vial for Lab & Vet MedicineNewsAug.14,2025
-
Premium Clear Plastic Vaccine Vials for Lab & Vet MedicineNewsAug.13,2025
-
Plastic Clear Vaccine Vials | Lab & Vet Liquid StorageNewsAug.12,2025
-
Secure 250ml Blue Plastic Vaccine Vials for Lab & VetNewsAug.11,2025