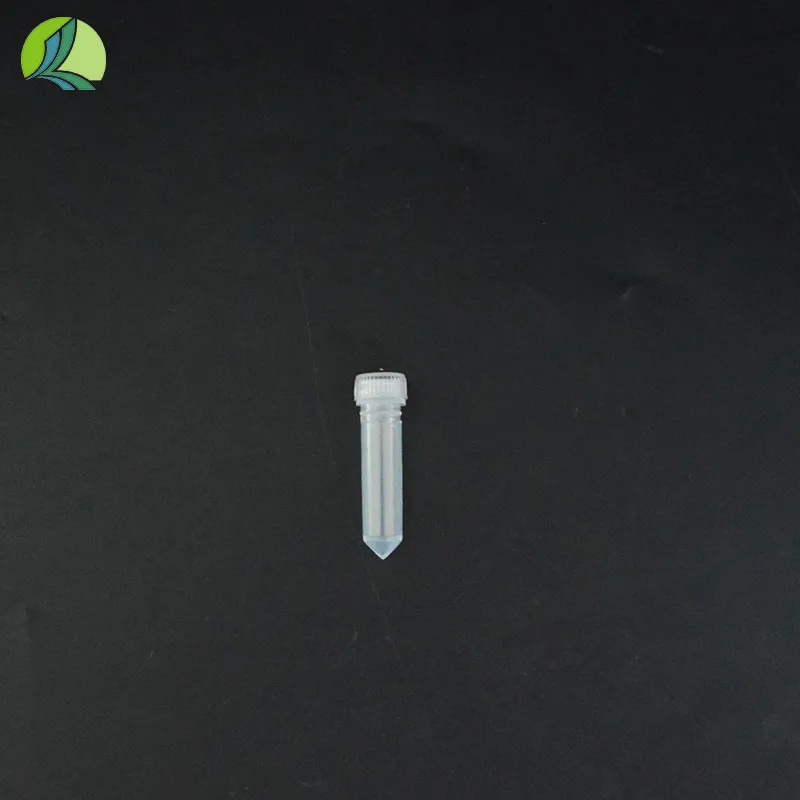
urine collection tubes with preservative
Urine Collection Tubes with Preservative Ensuring Accurate Diagnostic Testing
Urine testing is a vital component of modern medicine, providing essential insights into a patient's health. The introduction of urine collection tubes with preservatives has significantly improved the accuracy and reliability of urine sample analysis. These specially designed tubes are essential in preserving the integrity of urine specimens, preventing degradation, and maintaining the chemical composition necessary for accurate diagnostic results.
Traditional urine collection methods often leave samples vulnerable to contamination and degradation. Factors such as temperature fluctuations, exposure to light, and the presence of bacteria can alter the chemical composition of the urine, potentially leading to inaccurate test results. To address these challenges, manufacturers have developed urine collection tubes that contain preservatives. These preservatives act to stabilize certain components of urine, ensuring that the samples remain consistent from the time of collection to laboratory analysis.
There are several types of preservatives commonly used in urine collection tubes. One of the most popular is sodium borate, which helps maintain a stable pH and prevents the breakdown of substances such as urea and ammonia. This is crucial for tests evaluating renal function and metabolic disorders. Another commonly used preservative is acid, which can prevent bacteria from flourishing in the sample, an essential factor in maintaining the integrity of urine cultures. Additionally, some tubes may include stabilizing agents that preserve specific analytes, such as hormones or drugs, allowing for more reliable therapeutic drug monitoring.
urine collection tubes with preservative

The use of urine collection tubes with preservatives is especially important for timed urine collections, such as 24-hour urine tests. These tests require that all urine produced over a 24-hour period be collected for analysis. Given the extended collection time, it is critical that the samples remain stable. Tubes with preservatives minimize the risk of alteration during the collection process, allowing for an accurate assessment of the patient’s renal function, protein metabolism, and electrolyte balance.
Another key advantage of using urine collection tubes with preservatives is that they can streamline the testing process. When urine samples are collected without preservatives, they often require immediate refrigeration or prompt transportation to the laboratory to prevent degradation. This can be logistically challenging and increases the likelihood of sample rejection due to improper handling. In contrast, urine collection tubes with preservatives allow healthcare providers more flexibility in processing and transporting samples while ensuring that the results remain reliable.
The adoption of urine collection tubes with preservatives has vast implications for clinical practice. Not only do these tubes enhance the accuracy of laboratory tests, but they also improve patient care by providing timely and reliable results. Clinicians can make more informed decisions based on accurate diagnostics, leading to better patient outcomes and streamlined treatment plans.
In conclusion, urine collection tubes with preservatives represent a significant advancement in the field of diagnostic medicine. They play a crucial role in maintaining the integrity of urine samples, thereby safeguarding the accuracy of laboratory analyses. As healthcare continues to evolve, embracing innovations that enhance diagnostic accuracy is essential. The integration of preservative-containing urine collection tubes should be a standard practice across clinical settings, ensuring that both healthcare providers and patients benefit from reliable and precise diagnostic results. By prioritizing the quality of urine samples, the medical community can continue to improve patient care and health outcomes.
-
Aesthetic Makeup Spray Bottles | Fine Mist Empty RefillableNewsAug.19,2025
-
White Plastic Veterinary Vaccine Vials | Lab Liquid BottlesNewsAug.18,2025
-
Plastic Medicine Liquid Bottle: Secure Flip Top Drug VialsNewsAug.17,2025
-
Durable 250ml Blue Plastic Vaccine Vial for Lab & Vet UseNewsAug.16,2025
-
Sterile Virus Sample Tubes: Secure & Reliable Specimen CollectionNewsAug.15,2025
-
White 250ml Plastic Vaccine Vial for Lab & Vet MedicineNewsAug.14,2025